By Dr. Leo Montejo
Few have looked medically at the deaths on Everest this season. While some have reasonably cited hypoxia or cerebral or pulmonary edema as the causes of death, most sources claim that the victims perished from “exhaustion” after a long summit day.
Exhaustion is not a diagnosis in medicine. No coroner puts this on any document. While a long summit day is extremely demanding on the body, we need to be more precise about what this term means. It can be:
- Hypoxia from oxygen tank depletion
- Hypoxia from a poorly fitting mask or leakage
- Hypoxia from an inadequate flow rate of O2
- Hypoxia from regulator or mask failure
- Hypoxia from High Altitude Pulmonary Edema
- Dehydration
- Increased blood viscosity (elevated hematocrit) plus dehydration leading to stroke
- Cardiac arrhythmia
- Electrolyte imbalance
- Hypoglycemia
- High Altitude Cerebral Edema and collapse
- Hypothermia

In medicine, before a surgical procedure, we examine the patient to minimize risks. This sometimes includes an extensive cardiac exam, a treadmill test or even a coronary angiogram and clearance from a cardiologist. The heart tolerates risks poorly, and if there are any red flags, the operation is often postponed.
Other elements of a pre-op exam include lab tests and of course, a physical. The anesthesiologist also knows all medications that the patient is on.
To my knowledge, not a single expedition follows a stringent pre-climbing protocol similar to what we do in medicine. And on the mountain, climbers are not monitored the way one is during a surgical procedure. So let’s not be surprised with these deaths, which some are calling exhaustion.
Fatalities are probably due to:
- Hypoxia, which brings either collapse from lack of oxygen to the brain or cardiac arrhythmias, which we often see in medicine during hypoxic episodes: The heart, like the brain, does not like low-oxygen situations. This can also occur at night inside a tent, while the climber is sleeping. Lying flat causes shallower breathing, and the intestines also push up, collapsing some of the lungs. Together with a lower SpO2 (less oxygen in the blood), this can be fatal.
- Arrhythmias leading to cardiac arrest from hypoxia, dehydration or electrolyte imbalance. The heart is very sensitive to changes in potassium or calcium levels in the blood, and a long summit day can alter these dramatically.
- Hypoglycemia –- low blood sugar — can also lead to collapse. This could come after a long day without much food or from diabetes medications taken without food.
- Interactions between the medications that the patient is on, combined with the hostile environment. Many climbers on these expensive commercial expeditions are over 50 and may be on medications for high blood pressure or prostate drugs that can cause a severe drop in blood pressure and fainting. We have no data on this.
- Dehydration leading to elevated heart rates, low blood pressure and possibly stroke due to viscous blood.
- Hypothermia. While lethal, this also leads to tissue hypoxia earlier than expected. This is because at low temperatures, hemoglobin does not release oxygen to tissues as well as at normal temperatures. So even if you have enough oxygen in the blood, this oxygen may not be reaching your brain or other organs.
How is this tied to what happened on Everest this year?
- Long lines and wait times drained oxygen tanks.
- Long waits caused dehydration, which in turn led to very high heart rates and possibly tachyarrhythmias or even heart attacks.
- Long waits could also lead to hypoglycemia due to an extended day on the mountain.
- Long waits could bring on cerebral or pulmonary edema: In trying to conserve his oxygen tank, the climber reduces the flow without knowing whether what setting to use. (In medicine, we measure SpO2 continuously to make these types of decisions.)
- The fewer resources an expedition devotes to each client, the more problems will arise. If a climber has too little oxygen, water or calories, he will eventually collapse.
- There was no monitoring of SpO2 at night above certain altitudes.
- The well-publicized comment that 50% of climbers will have a problem on Everest is completely irresponsible. Surgery is also dangerous, but we take all sorts of measures to prevent complications.

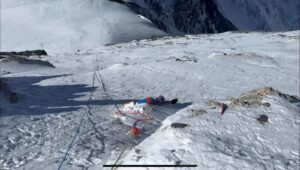
A rescue on Everest.
Recommendations
In medicine, we have Standards of Practice. In the United States, for example, these are defined ( in the case of surgery) by the American Board of Anesthesiology. They determine what a pre-operative exam should contain and define minimum monitoring standards for patients. Similar standards need to be set up for 8,000m commercial expeditions, including:
- How much O2 is available per climber per expedition.
- How many Sherpas or porters are available per climber.
- What type of pre-expedition medical exam should be mandatory for different ages. Requirements are not the same for a 30-year-old and a 50-year-old.
- What medical back-up is needed for each expedition.
- What monitors climbers will wear. Heart rate and SpO2 monitors are ideal and will prevent many complications. [Full disclosure: I am affiliated with a company that offers such monitoring devices.] Also, keeping heart rates below 130 and SpO2’s above 80% at all times will ensure greater safety.
About the author: Dr. Leo Montejo did his residency at Harvard in anesthesiology and critical care medicine and is a former professor at Stanford in this specialty. He is an extreme sports enthusiast and has participated in five Himalayan expeditions.