Although we live in an age with unrivaled access to information, climbing statistics don’t typically include the number of injured climbers each season. It is hard to know, for example, how many return each year with one more summit but one or more fewer toes. How common is frostbite, and what are the consequences?
Dr. Monica Piris has seen a lot of frostbite over her 20 Himalayan trips as an expedition doctor. Fourteen of those trips were to 8,000’ers, 10 of them to Everest Base Camp.
“In my personal opinion, losing a digit to frostbite is a sign that something went horribly wrong on a climb,” she told ExplorersWeb. “I would never call a climb a success if the climber sustained frostbite.”
We spoke to Dr. Piris about symptoms, treatment, and how much supplemental O2 reduces the risk of frostbite.

Monica Piris treats a patient during an Ama Dablam expedition. Photo: Courtesy of Monica Piris
Unrecognized risk
Do high-altitude climbers underestimate the risk of frostbite?
There is a huge lack of knowledge about cold injury among people attempting 8,000m peaks. [Frostbite] is actually more of an unrecognized risk than an underestimated risk.
There is a lack of knowledge about how to prevent it, what to do if it happens, and how truly life-changing losing a digit can be. This lack of understanding leads to an inability to calculate the risk involved, as well as an inability to judge the severity. It’s basically the worst of all worlds.
On 8,000m peaks, supplementary oxygen is widely available and used for longer periods at lower altitudes at higher flow rates than ever before. How has this helped limit frostbite?
I don’t have access to exact numbers, but my impression is that although you might think an increase in the use of high-flow oxygen helps prevent frostbite, that is not necessarily the case. The huge increase in the total number of people going up (and the relative lack of experience of those people) has meant that the total number of cases per year has remained the same or even increased.
However, I would guess that the number of cases per 1,000 climbers may have decreased and that would likely be a result of high-flow oxygen use.
Less oxygen, more risk
A number of clients on commercial expeditions have announced that they plan to climb without bottled O2. What should they be aware of?
For climbers used to supplementary oxygen, it is important to realize that the weather windows appropriate for climbing with oxygen may not be suitable for a no-O2 attempt. The first important decision in preventing frostbite is to know when the conditions are too severe for a safe attempt without O2.
Climbers going above 8,000m without supplementary oxygen face many challenges. One of these is the inability to generate enough heat to keep their core temperature up and to stop their extremities from freezing. Not only is heat generation a problem, but heat loss is much more significant because of the increased rate and depth of breathing.

Kristin Harila has announced plans to summit all 14×8,000’ers without supplementary O2, after reaching the top of 12 of them aided by bottled gas. Photo: Kristin Harila/Facebook
No margin for error
Those attempting a no-O2 climb need to understand how much more at risk they are of sustaining a cold injury. They should be constantly thinking about their fingers, toes, cheeks, and nose. To me, that means a regular mental check: Can I feel all my toes? Can I feel my fingers? Almost like an hourly mantra. If the answer is ever no, they need to stop, check, rewarm, or turn around.
The margin for error when climbing without oxygen is so close to zero that missing the moment at which you should turn around almost always has significant consequences. Knowing when it’s OK to keep pushing versus when it’s a potentially fatal error is something that comes from experience. Ill-placed, inflexible motivation is a dangerous thing.
One common mistake is removing a glove to fiddle with a camera or a carabiner. Skin contact with a cold metal object can cause a direct freezing injury to that patch of skin. Even that momentary removal of protection might make it very difficult to get that hand warm again.
Frostbite can happen almost anywhere
We are used to seeing frostbitten climbers on their return from a summit, but what about trekkers? Are they safe from frostbite at lower altitudes?
Cold-related injuries, including frostbite, can occur at sea level if the temperature is low enough. The low partial pressure of oxygen in the air at altitude makes it much more likely because our ability to generate heat is so impaired by the lack of oxygen. The small amount of blood that does reach the extremities carries very little oxygen, so metabolic processes that generate heat are almost at a standstill.
Yet freezing temperatures alone cause cold injury and can happen anywhere. There are many cases of urban frostbite, often affecting vulnerable people in cities where the winters are severe. So yes, trekkers can also sustain frostbite.
Note that the actual air temperature must be below freezing for frostbite to occur. Wind chill equivalents do not count. Near the summits of 8,000m peaks, however, it’s always below freezing.
Symptoms
So, which symptoms do we need to pay attention to, and what should we do if they appear?
If you’ve felt cold for a while, then ask these questions:
Can I feel all my toes?
Can I feel all my fingers?
Can I feel the tip of my nose and ears?
If they are numb or feel wooden, this is a sign that you need to act. That might be doing windmills with your arms, wiggling toes, or gently rubbing your ears/nose. If this doesn’t work and the feeling doesn’t return, then the climber should turn around and descend to a place of relative safety to focus on rewarming their numb extremity.
If the climber has access to bottled oxygen, then putting it on will immediately improve the blood flow and will warm their extremities.
Finally, if an extremity remains numb for too long, it is likely frozen. Freezing of the intracellular and intercellular fluid causes irreversible structural damage to the cells which results in tissue death and the need for amputation. This is what frostbite is.

Amisha Chauhan of India suffered frostbite after being caught in traffic jams near the summit of Everest in 2019. Photo: DNA India
Frostbite means something has gone very wrong
Some climbers are motivated to endure hardships. That might push them to keep climbing and ignore symptoms. To reach the summit, some may believe the possibility of losing a toe or a fingertip is a risk worth taking. What is your advice for such diehards?
In my opinion, losing a digit to frostbite is a sign that something went horribly wrong on a climb. I would never call a climb a success if the climber sustained frostbite.
I think a lot of people hugely underestimate the impact of losing a piece of a finger or toe. The way we walk depends on having five full toes. To lose even just a piece of one toe entails months of pain followed by having to learn how to walk again.
Frostbite risk higher for no-O2 climbers

14×8,000m climber Juan Oiarzabal was so seriously frostbitten on K2 in 2008 that he lost all toes. Photo: El Correo
Minimizing heat loss

David Goettler wearing an AirTrim mask. Photo: David Goettler
Treatment in the field and afterward
How is frostbite treated?
The treatment of frostbite can be usefully divided into what you can do in the field and what needs to happen in a hospital.
In the field, administer oxygen as soon as possible, if it is available. Hot sugary drinks will help elevate the core temperature and blood glucose. Once in a place of safety, and once you have confirmed that there are no other injuries, concomitant hypothermia, or other life-threatening altitude illnesses, then remove all layers and inspect the affected body part. If it is frozen, it will be white, cold, and hard, like a piece of frozen chicken.
The next step is vital. You need to think about getting to an evacuation point. If you have a frozen foot, but you need to wear your boots to descend for evacuation, then you should not start rewarming. Rehydrate, rest, then continue your descent as soon as it is safe to do so.
The reason for this is twofold: First, if the affected body part refreezes after being warmed, the damage will be much more severe. Second, if it is a foot or toes, the swelling that will occur after rewarming will make it impossible to put a boot back on, and walking will be impossible. It is better for the extremity to remain frozen until the climber arrives at a place where evacuation assistance is possible.

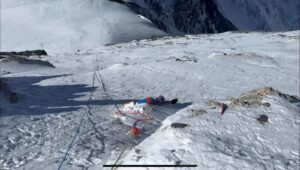
Treating frostbite in a Base Camp tent. Photo: Basque Country’s Mountain Federation
Rewarming: care needed
When rewarming in the field, use warm water at no more than 37ºC in a basin that is large enough to submerge the affected body part without touching the sides. Add a capful of iodine to the water. Once the frozen body part is in the water, the water cools very quickly, like when you put an ice cube in a drink. It is necessary to regularly add more 37ºC water. Take great care when adding hot water as the frozen part is unable to feel anything and can easily be burned.
Once rewarming is complete, the foot or hand will feel warm and soft. There will be redness and swelling will become apparent. Blisters may appear. There is likely to be an awful lot of pain which will need aggressive treatment with painkillers.
There is evidence to support the use of low-dose ibuprofen (200mg per day). If the patient is still at high altitude, research shows that supplementary oxygen and the use of a portable hyperbaric chamber can minimize damage. Aloe vera gel, soft, bulky, protective dressings, and elevation of the whole limb are about all that is possible in the field.
Long-term care
Within 72 hours of rewarming, the victim should be evacuated to a hospital where doctors can administer Iloprost intravenously. Iloprost is a medication that several small studies have shown can reduce the need for amputation in digits affected by frostbite.
However, its use with acute frostbite is not permitted in all countries (in the U.S., for example, it is not allowed). Usually, intravenous infusions of iloprost are given for five consecutive days before the patient can make their way back to their home country for ongoing care over subsequent weeks.
It is important that a surgeon (usually a vascular surgeon) with experience and knowledge in the treatment of frostbite provides ongoing care. The affected digits need to be left for several weeks, with great precautions to avoid infection. During this process, all the dead tissue eventually turns black and shriveled.
It is truly devastating, and patients who have suffered these injuries usually agree that these weeks of waiting are the hardest. They must watch their fingers or toes turn black, shrink, and sometimes fall off.

Blisters caused by frostbite. Photo: Basque Country’s Mountaineering Federation
There are two reasons why it is recommended that this process happen naturally rather than immediately having surgery. First, the body will make it very clear where the line of surviving tissue is. If we jump in with surgery too soon, it is almost always at the expense of some viable tissue.
Second, some surgery to tidy things up is almost always necessary. The longer we allow the tissue at the edge of a frostbitten digit to repair itself, the better it will withstand this final surgery.

Frostbite can happen anywhere the temperature is below freezing. Above, a Russian polar traveler lost two toes to frostbite on one Arctic Ocean expedition. Photo: Jerry Kobalenko
Final thoughts
There is another medication, Tissue Plasminogen Activator (TPA), which doctors can also use in the acute treatment of frostbite. However, the window for administering this is just 24 hours, so it is almost impossible in the context of most climbing or remote adventure injuries.
Finally, there is also some recent anecdotal evidence that hyperbaric chambers may be helpful in reducing subsequent tissue loss. But as yet, there is no quality scientific evidence to support this.
Dr. Monica Piris (MBChB, Dip. Mountain Medicine) has worked as a doctor on high-altitude expeditions since 2007. She has been on more than 20 expeditions to the Himalaya, including 14 to 8,000m peaks. She now works as the expedition doctor for Alpenglow Expeditions and offers medical coverage for private expeditions. When not on an expedition, she divides her time between her home life in northern Spain, Chamonix, and the UK, where she works part-time in emergency medicine. She is the partner of mountaineer David Goettler, whom she first met at Everest Base Camp.

Monica Piris during an Ama Dablam expedition. Photo: Courtesy of Monica Piris